Centering people in primary health care
Transforming siloed approaches into person-centered, integrated services.
Advocacy and Public Policy
Digital Health
Early Childhood Development
Epidemic Preparedness and Response
Gender
Health Systems
HIV/Tuberculosis/Viral Hepatitis
Human-Centered Design
Maternal, Newborn, Child Health and Nutrition
Noncommunicable Diseases
Sexual and Reproductive Health
Vaccines

Dr. Ali Kitoko shares information on an HIV self-test at Pharmacie Binamet, 1 of 28 pharmacies in Haut-Katanga Province, Democratic Republic of the Congo, to introduce pharmacist-assisted HIV self-testing services during COVID-19. Photo: PATH/Raphael Mwam.
The challenge
Primary health care (PHC) should provide the most basic package of essential health services and products. It spans a person’s lifetime, covering about 80 percent of their health needs throughout their life, from services for things like childhood immunizations, nutrition, and COVID-19 to HIV, reproductive health, malaria, oxygen, and cancers, and is the “expressway” to achieving universal health coverage.
PHC systems are central to health equity. At every stage of life, access to integrated, person-centered care enhances a person’s overall health and well-being because how care is delivered determines if PHC services are actually accessible to individuals and communities.
The solution
Integrated, person-centered care means putting people and communities, not diseases, at the center of health systems. It means making multiple services available in one place so care is easier for people to access. It helps minimize health system fragmentation, fosters collaboration between public- and private-sector providers, and delivers organized health services that better meet people’s needs.
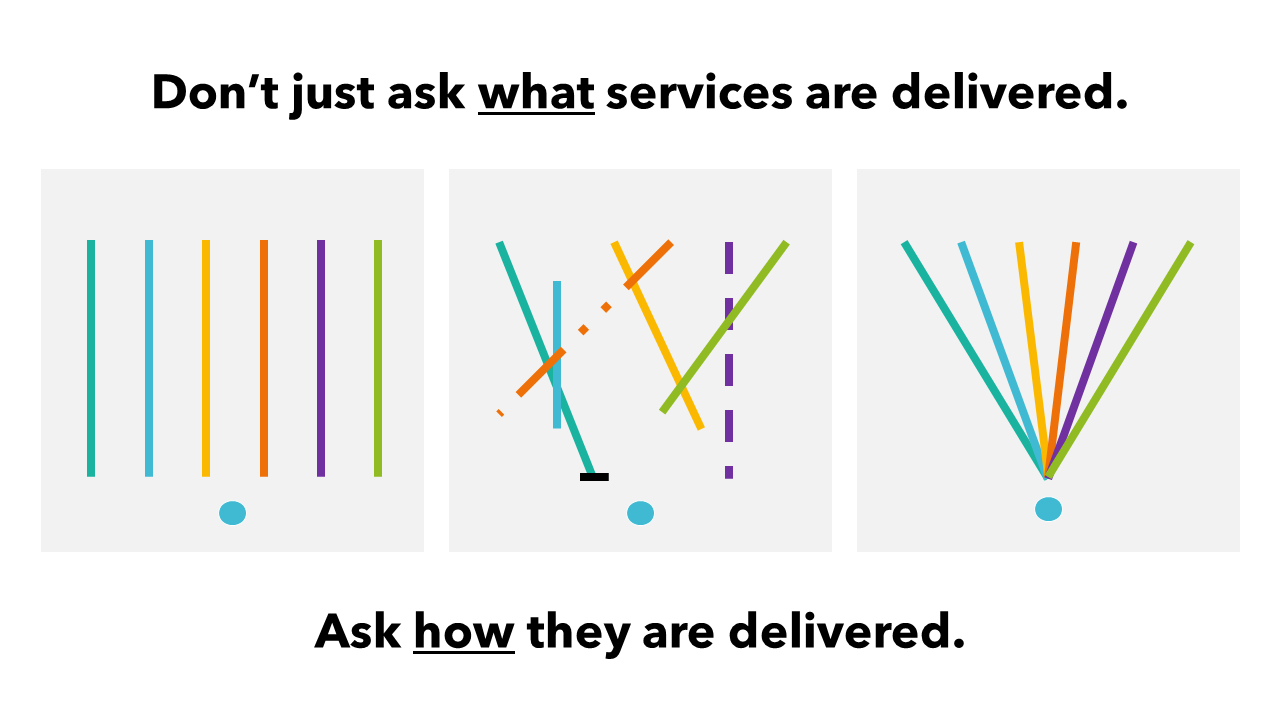
Just because multiple services are offered does not necessarily mean they'll be accessible. Integrating services at the point of care is a proven way to improve both access and outcomes. Image courtesy of Primary Health Care Performance Initiative.
Why was PATH chosen to do this work?
PATH is uniquely positioned to drive PHC impact. Working in more than 70 countries, we have firsthand knowledge of the issues and contexts in which we work, and we take a holistic approach to a patient’s life cycle.
Our PHC program is made up of a multidisciplinary team with deep technical expertise in early childhood development; HIV, tuberculosis (TB), and viral hepatitis; maternal, newborn, child health and nutrition; noncommunicable diseases; and sexual and reproductive health; and health systems.
We deploy crosscutting approaches to make an impact. PATH engages policymakers, influencers, and civil society to ensure PHC is prioritized, and we are thought leaders in the digital transformation and use of data in PHC systems. We apply a health market lens to improve equitable access to essential health products and services, and we use human-centered design to co-design solutions with our partners based on their lived experiences.
“Our PHC approaches have shown improved health outcomes, more targeted investments, and more resilient health systems.”— Kimberly Green PhD, Global Program Director, Primary Health Care, PATH
Our approach
Evidence underscores that offering a range of essential health services with effective case management and multidisciplinary teams leads to better outcomes and less expensive care (the World Health Organization has explicitly called for this shift). Public-private partnerships, task-shifting, differentiated service delivery models, and self-care can all help to accelerate delivery of integrated, person-centered PHC and enhance access to and coverage of high-quality care and coverage.
Since the launch of our PHC program in 2021, PATH has focused on—and found great success in—working with ministries of health to advance integrated, person-centered, PHC using five intersecting approaches:
- Starting from what people need and want.
- Creating opportunities for greater integration in routine and chronic disease systems and services.
- Partnering with communities and health leaders to deliver responsive care to populations left out of mainstream services.
- Increasing access to affordable self-care approaches and tools.
- Making system-wide changes that reinforce integrated care.
1. Starting from what people need and want
Standardized health packages can be important in determining what gets covered at each level of care, but to be effective they must be paired with a more contextualized understanding of other factors like culture, epidemiology, and the localized impacts of climate change. These nuanced factors aren’t so easily addressed through standardized packages, but they have a big impact on health care access and uptake.
That’s why at PATH we help stakeholders determine where changes are needed in service packages and system designs using a combination of human-centered design, triangulated data, quality improvement collaboratives, and community-led decision-making. Through this approach, we’re able to align the services offered with what people truly need and want.
For example, since 2021, PATH’s team in Zambia has worked to develop and refine innovative, person-centered service delivery models for integrating family planning information and services into routine childhood immunization programming. The focus is on reaching rural, postpartum women who wish to space or limit births and who rarely interact with the health system. To identify nuances and develop practical solutions, PATH’s Living Labs team hosted human-centered design sprints with postpartum women, male partners, and traditional and faith leaders as well as health leaders in PHC, family planning, and immunization. Together, we’re reimagining integration of these services and identifying ways to more holistically meet the needs of mothers and infants.
2. Creating opportunities for greater integration in routine and chronic disease systems and services
Siloed health funding has advanced targeted goals like reductions in the prevalence of an infectious disease, but that narrow focus has left some countries with difficult decisions about resource allocation for other important health areas. In the Democratic Republic of the Congo, Ghana, India, Kenya, Mozambique, Ukraine, Vietnam, and Zambia, PATH helps local partners offer integrated services that break down barriers to access at the service delivery point.
For example, when COVID-19 vaccination began in Ghana, PATH provided hypertension screening at vaccination clinics. “This was an optimal moment to reach an older population more at risk for hypertension,” says Robert Yeboah, MD, Senior Technical Advisor for Noncommunicable Diseases. “And it’s been successful: we’ve screened more than 20,000 people and linked 1,401 to care in early 2021.”

The PATH-supported Healthy Heart Africa program leverages COVID-19 vaccination campaigns to expand hypertension screenings in the Ashanti Region of Ghana. Photo: PATH/Robert Yeboah.
In Mozambique, PATH assisted the Maternal and Mental Health Departments at the Ministry of Health to develop and pilot the country’s first-ever protocol for screening and managing postpartum depression (PPD) within routine postnatal care. Instituted in eight health facilities in Maputo Province, the pilot showed the effectiveness of integrating mental health screening for new mothers. When a case of potential PPD was identified, a mental health provider followed up with the mother. More than 70 percent of suspected cases of PPD referred by nurses were confirmed by mental health technicians.
3. Partnering with communities and health leaders to deliver responsive care to populations left out of mainstream services
PATH’s strong partnerships with national and subnational governments, civil-society groups, and private-sector actors position us to meet the evolving needs of individuals and communities, especially during times of change.
Since the war in Ukraine began in February of this year, 12 million people have been displaced. Through our US Agency for International Development TB and HIV projects, we’ve used mobile care delivery to support the local PHC system in bringing health services and information about health threats closer to people. In ten regions with large populations of internally displaced persons (IDPs), we conducted risk assessments of, and interviews with, IDPs and administered medical examinations and vaccinations not only for COVID-19, but also for tetanus, diphtheria, polio, and measles, mumps, and rubella.
In Vietnam, PATH’s Healthy Markets program supported the development and launch of sustainable one-stop-shop clinics to offer key populations a suite of integrated services, including HIV testing, pre-exposure prophylaxis (PrEP), antiretroviral treatment, and services for TB, viral hepatitis, sexually transmitted infections, noncommunicable diseases, mental health counseling, and addiction management. These social enterprise clinics are led and owned by key populations themselves, whose services are valued by local health authorities for enabling greater health care coverage and choice. This represents a smart and effective partnership between the Ministry of Health and communities in leveraging unique capabilities to help achieve universal health coverage by 2030.
Over a 14-month period, these integrated clinics boosted access to essential health services for 12,624 key population clients. For those seeking PrEP or antiretroviral treatment, more than half obtained additional services at the clinic, and 38 percent of clients who came in for non-HIV services were subsequently linked to HIV testing and/or PrEP. Addressing mental health morbidity also increased clients’ continuation in PrEP services.
4. Increasing access to affordable self-care approaches and tools
Person-centered care includes improving the ability of people to self-manage their health more effectively. In Ukraine, India, and Vietnam, PATH is advancing digital adherence technologies and smartphone apps to support people with TB to complete their course of treatment. These tools support health promotion and engagement among those living with single or multiple chronic conditions. In the Ukraine pilot, use of digital adherence technologies helped 83 percent of patients take more than 95 percent of planned doses.
We are also rolling out bundled self-care approaches tailored to the needs of different population segments, including adolescent girls and young women, key populations, and people living with diabetes. In several countries in Africa, PATH is using human-centered design to achieve a co-bundling solution that makes diabetes self-care easier for the thousands of people who struggle to safely manage the disease.
In Uganda, co-packaging of family planning, HIV self-testing, and menstruation products is enhancing discreet access to key sexual and reproductive health services among girls and women. Also, an online platform in Vietnam offers HIV and COVID-19 testing and prevention tools to those in need.
In Senegal, the Ministry of Health, PATH, and a coalition of partners developed the first national self-care guideline in francophone Africa, covering a wide range of self-care interventions in the areas of reproductive health and family planning, prenatal and postnatal care, noncommunicable diseases, and sexually transmitted infection and HIV prevention, screening, and treatment.
5. Making system-wide changes that reinforce integrated care
Ultimately, reforms in policies, structures, and financing are required to reinforce and sustain integrated person-centered care. This includes addressing integration as part of health system building blocks.
PATH is undertaking a landscaping review of PHC policies to understand the policy ecosystem in over 25 countries, including how national-level policies and strategies articulate the critical components of a strong and well-functioning PHC system. This analysis will help ascertain what services are contained within the remit of PHC, which workforce is assigned to PHC, and if there are unified or fragmented supply chains and financing. To inform advocates, policymakers, and other partners on where there might be additional opportunities to reform PHC policies and systems, a dashboard visualization tool can be explored to inform the next policy design process and help to ensure barriers to advancing integrated PHC are addressed.
In Uganda, PATH partnered with the Ministry of Health to assess PHC financing at national and subnational levels between 2016 and 2020, ultimately contributing to a 7 percent increase in the PHC national budget in 2020. In Kenya and India, a major effort is underway to develop policies that encode strong PHC systems and support their effective implementation.
In Kenya, PATH’s Advocacy and Public Policy team provided technical assistance to the Ministry of Health to adopt policies for PHC. Among these was the Primary Health Care Network (PCN) Guidelines, which lay the foundation for the implementation of PHC in the country. The guidelines emphasize integrated care and moving from the current curative focus to a preventive, person-centered approach, ensuring a greater return on investment—because for every dollar invested in PHC, Kenya will save 14 dollars. The PCN model is being implemented as an integrated approach to service delivery, with community health care, dispensaries, and health centers serving as spokes linked to a hospital, which serves as the hub, overseen by a multidisciplinary team at the subnational level.
“PCNs are a way of linking and strengthening health care services through building on a person-centered approach to health,” says Patrick Amoth, MMeD, Ag. Director General for Health with Kenya’s Ministry of Health. “This enables provision of proactive, personalized, coordinated, and integrated social and health services.”
The results
Investment in high-quality, person-centered care pays dividends to patients, health care workers, and country economies alike. When PHC systems and services are intentionally designed for integration based on community need, their ability to reach and address individual health concerns improves. Here are just a few of the results from 95 PHC projects across 50 countries.
Partners
PATH is proud to partner in this work with the governments and health ministries of the DRC, Ghana, India, Kenya, Mozambique, Senegal, Uganda, Ukraine, Vietnam, and Zambia; as well as Allies Improving PHC; Bill & Melinda Gates Foundation; Global Fund to Fight AIDS, Tuberculosis and Malaria; Unitaid; US Agency for International Development; and World Health Organization.
Resources
- Using Behavioral Science & Human Centered Design to Boost COVID-19 Vaccination: Insights and Strategic Interventions
- HIV Self-Testing: Increasing access by optimizing quality, choice, and convenience
- Assessment of the integration of postpartum depression screening and counseling into primary health care in Mozambique
- Let’s Talk About Mental Health: Integrating care for depression, anxiety, and substance use as a part of HIV services in Vietnam