Editor's note: SARS-CoV-2 variants have been making headlines for months—from alpha (first detected in the United Kingdom) to delta (discovered in India this spring) to lambda (currently driving case counts in Argentina, Brazil, Chile, Colombia, Ecuador, and Peru). Understandably, these variants have raised concerns about the continued efficacy of COVID-19 vaccines.
A recent analysis, published in the New England Journal of Medicine, compared the rates of infection with the two variants that caused the second and third COVID-19 waves in England according to vaccination status. The data suggests that two doses of COVID-19 vaccine provide a strong protective effect against both variants—as much as 87.5 percent against alpha, and 79.6 percent against delta.
A recent paper, raises some concerns on the ability of hte lambda variant to evade immunity. The authors suggest that mutations to lambda's spike protein have made it more transmissible and about 1.5 times more proficient at escaping the neutralizing antibodies elicited by vaccination in laboratory tests—which may account for lambda's rise in countries like Chile, where as much as 60 percent of the population had received a single vaccine dose.
As new variants continue to emerge—and bodies of evidence about them continue to grow—we can look to other viruses to understand the relationship between virus variants and vaccine efficacy. In this article PATH rotavirus expert Miren Iturriza-Gomara, PhD, shares insights from her research on rotavirus variants.
* * * * *
As a virologist working at PATH, I focus on rotavirus: a leading cause of severe and fatal diarrheal disease in young children, and a long-time subject of virus variant research.
With SARS-CoV-2 variants making global headlines, we can look to rotavirus for important lessons about virus variants and vaccine efficacy.
1. Viruses evolve. It’s what they do.
The existence and continued emergence of virus variants is normal for all viruses.
Changes in the virus genome, called mutations, occur at random as they multiply. Mutations can have a big or small impact, and can affect the survival of the virus, its ability to adapt to new hosts, its transmissibility, disease severity and characteristics—even its ability to escape recognition by antibodies generated after previous infections or vaccination.
Rotaviruses are very diverse. They are classified into types depending on the composition of the two proteins that make up the virus’ external layer.
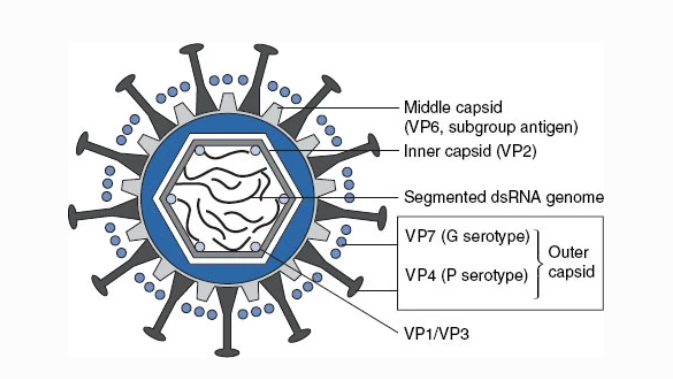
The ’G’ and ‘P’ proteins on the outer layer (capsid) of rotavirus vary by rotavirus type. Image: Grimwood, Lambert, Milne.
The distribution of rotavirus types varies significantly between different countries and regions of the world—and within the same region from one year to the next. However, regardless of type, all rotaviruses cause the same disease, and no type has been associated with more severe symptoms.
2. Rotavirus variants have little effect on vaccine efficacy, regardless of vaccine type.
The oral rotavirus vaccines currently in use have been developed using two different general approaches. One approach relies on the vaccine containing one variant: either a weakened version of the most commonly circulating virus variant, or a variant that caused asymptomatic infection in newborn infants.
This approach assumes the single variant will provide sufficient cross-protection against other rotavirus variants. A second approach relies on the vaccine having a combination of the most frequently found variants, with the goal of developing greater variant-specific protection.
Virologists like me have been studying the global diversity of rotaviruses in order to monitor whether vaccination influences the virus’ diversity. The aim is to investigate whether some rotavirus types may be found more frequently in vaccinated children, as this could indicate either that the vaccine does not protect—or protects less effectively—against a particular rotavirus type.

Year-to-year change in distribution of the six most frequently found rotavirus types in 11 countries across Europe. Image: EuroRotaNet.
Researchers do this by comparing the diversity and types of rotaviruses found in children with diarrhea before and after rotavirus vaccination is introduced in a population. We also evaluate the diversity and types of rotaviruses causing disease in vaccinated versus non-vaccinated children in the same region of the world.
Overall, the rotavirus diversity and evolution data we have been studying for over a decade tell us that—like with natural infection—rotavirus vaccines produce a good degree of cross-protection against a variety of rotavirus types.
3. Monitoring strain diversity before and after vaccination campaigns provides crucial information.
Right now, PATH and partners are developing a new generation of rotavirus vaccines aimed at providing better protection for the children most affected by rotavirus diarrhea. As these new vaccines are developed, monitoring their effectiveness against different rotavirus types will remain crucial.
Without genetic surveillance, we cannot know what virus variants are circulating, how well interventions like vaccines are working against them, or how to change course if needed. I believe this will be crucial for COVID-19 vaccines as well.
4. Even with reduced efficacy, vaccines save lives.
Rotavirus vaccine efficacy is not identical against all strains—a greater degree of protection is offered against variants closely related to the vaccine virus, and a lesser degree against more distant relatives. But even with less protection, it is important to remember that rotavirus vaccines still protect children from severe diarrhea and death.
As with COVID-19 vaccines, even if the impact on infection and transmission varies by vaccine, location, and virus variant, rotavirus vaccines save many lives. Partial protection is always better than no protection—in many cases, it’s the difference between life and death.
A version of this article was originally published on April 5, 2021, and has been updated with additional COVID-19 variant information.



