Imagine this scenario: you have a severe stomach ache and your condition is deteriorating day by day. You get hospitalized and undergo treatment, but medications fail to cure your ailment or bring relief. Soon the doctors tell you that, of the eight different antibiotics that usually work to cure an E. coli stomach infection, none are working. A once easily curable infection has become untreatable for you, and it could even cause your death!
This terrifying situation is not a scene out of a sci-fi movie, it’s reality for thousands of people across the globe who are affected by antimicrobial resistance (AMR). Antimicrobial resistance develops when microorganisms present in our bodies change over time after being exposed to antimicrobial drugs, such as antibiotics. Microorganisms that develop antimicrobial resistance are sometimes referred to as “superbugs”.
Antimicrobial resistance: A global threat
Antimicrobials have saved millions of lives by curing infections and made possible organ transplants and other complex surgeries. However, over the last few years, microbes have gradually developed resistance, creating an emerging threat to public health.
Poor infection control practices and excessive and improper use of antimicrobial medicines in both humans and animals have transformed AMR into a major health concern worldwide. If the resistance continues to build at the current rate, we could revert to a world where simple infections are no longer treatable.
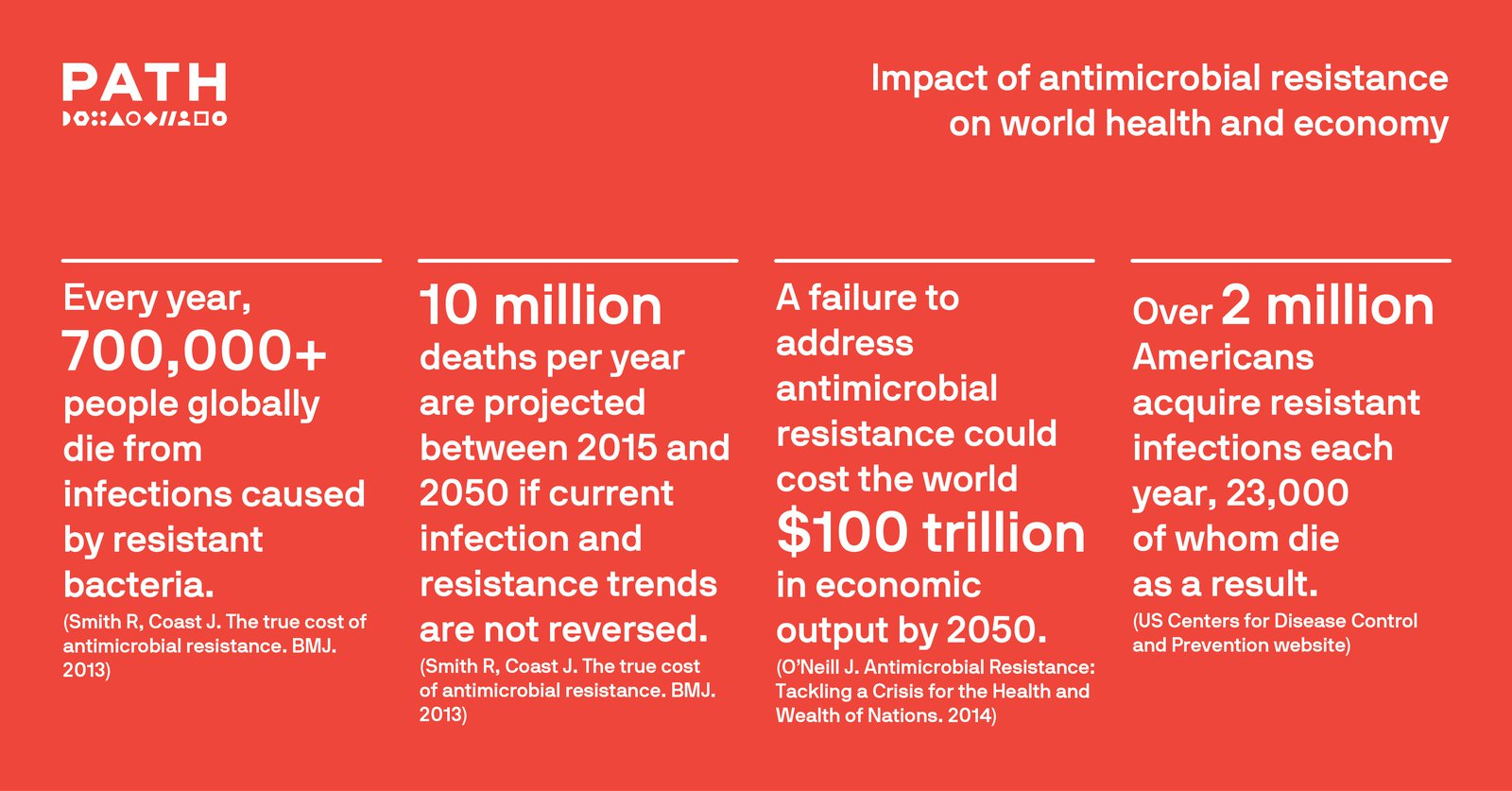
The direct impacts of AMR on health are severe, with increased morbidity and mortality in countries of all income levels. The consequences of AMR are grave and the public health community across the globe is now grappling with the question of how to collectively combat the emergence and spread of antimicrobial resistance before it develops into a hazardous pandemic.
In 2016, the United Nations General Assembly highlighted the potential crisis and called for global coordinated efforts to reduce AMR. The challenges faced in combating antimicrobial resistance are multi-faceted and multi-sectoral. According to WHO, antimicrobial resistance is a complex problem that affects all societies and is driven by many interconnected factors. Single, isolated interventions have limited impact. Coordinated action is required to minimize the emergence and spread of antimicrobial resistance.
PATH at the forefront of antimicrobial resistance control efforts
A leader in global health innovation, PATH is at the forefront of finding and implementing effective approaches to tackle AMR across the world. Our capabilities are optimized to provide a seamless end-to-end solution for countries developing new AMR response plans or building upon existing ones.

As part of a five-year commitment, through the Global Health Security Partnership (GHSP), PATH is supporting ministries of health and CDC in strengthening health systems and laboratories in the Democratic Republic of the Congo, India, Senegal, Tanzania, and Vietnam to better prevent, detect, and respond to public health emergencies and outbreak threats, including those related to AMR.
PATH is a member of the Northwest Antimicrobial Resistance Coalition, a U.S.-based group that creates and integrates effective interventions to stop antimicrobial resistance emergence and spread. With a focus on One Health approaches—which recognizes that people, animals, and their shared environment are interconnected—the coalition tracks the spread of antimicrobial resistance to provide a cohesive integrated system of global surveillance and support.
With support from the UK government through the Fleming Fund, PATH is working on AMR in Zambia, Vietnam, Kenya, and Sri Lanka. PATH’s India country program and Global Health Security Agenda program will be supporting the Government of Sri Lanka to tackle AMR. Under this project PATH will help to strengthen 16 human health and 4 animal health laboratories in Sri Lanka. PATH will also support the development of management guidelines for lab assessment and upgradation, and digitization of data to address the AMR needs of Sri Lanka. This is a key project to demonstrate AMR control in low- and middle-income countries and the learnings from this would be used for implementation in other countries.
International cooperation: A key element to combat antimicrobial resistance
The threat of antimicrobial resistance is a pressing public health issue that deserves the attention of the global health community. AMR cannot be addressed by any single organization or sector, that’s why international cooperation is essential. Communities are also invaluable partners in tackling this problem. By informing and engaging communities, the threat of AMR can be detected early and mitigated. The role of surveillance is therefore very important in tracking the occurrence and spread of AMR across communities.
Coordinated efforts, thus, will pave a path forward to address and contain this rising global health concern before it becomes a major health crisis, with no new antibiotics available and public health actions not fully implemented.
