Fifteen years ago, roughly two million children under age five died from pneumonia annually. Today, that number is down by more than half, thanks to improved prevention and treatment interventions and their growing presence in traditionally underserved countries.
Despite this progress, pneumonia still kills more children than any other infectious disease, especially in the developing world. Why? Because it is a complex disease with many causes and the tools to fight it are still not equitably accessible. To finish the job, we must harness an integrated array of solutions (vaccines, treatments, clean air, nutrition, and diagnostics) that can hit pneumonia from multiple angles.
Here’s my list of five particularly exciting solutions that are vital for enhancing the fight against pneumonia and overcoming systemic barriers that inhibit children from getting the prevention and care they need.

There are vaccines on the horizon that hold great promise to protect against all pneumococcal strains. Photo: PATH/Heng Chivoan.
1. Vaccines to provide broad protection
Vaccines against the leading cause of severe childhood pneumonia—pneumococcus—are effective against a number of the bacterium’s many varieties, but not all. They are also too expensive for many countries to afford without substantial donor assistance. By design, they’re doing their job, but what if a vaccine could provide affordable protection against all pneumococcal strains? The good news is vaccines designed to do just this are on the horizon. Public-private partnerships are advancing the development of vaccines that hold the promise to potentially change the pneumococcal prevention game.
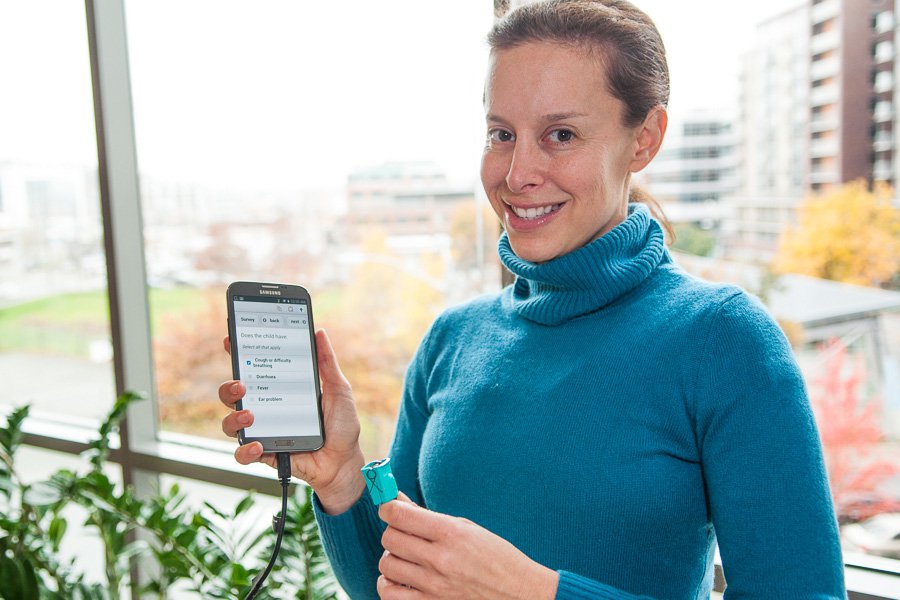
Dr. Amy Ginsburg demonstrates a user-friendly application for mobile phones and tablets called mPneumonia that aims to help health care providers detect and manage pneumonia. Photo: PATH/Patrick McKern.
“We must harness integrated solutions (vaccines, treatments, clean air, nutrition, & diagnostics) that can hit pneumonia from multiple angles.”
2. Technologies to diagnose and treat low oxygen levels
By afflicting the lungs, pneumonia can result in fatal oxygen deficiency. A pulse oximeter is the gold standard for noninvasively diagnosing this deficiency. It easily and painlessly clips on a finger or other extremity to measure blood oxygen levels, and it can inform the best use of lifesaving oxygen treatments. In low-income countries, however, supply, policy, training, and cost hurdles make pulse oximetry and oxygen scarce resources, particularly for children. Investing in creative ways to address the challenges (like mobile phone applications or alternative energy for pulse oximetry) is critical for expanding use.

Fast-dissolving tablets are an easy and cost-effective way to administer antibiotics to children. Photos: PATH/Patrick McKern.
3. Child-friendly antibiotics ideal for low-resource settings
The recommended first-line treatment for childhood pneumonia is the antibiotic amoxicillin. In its traditional forms, it’s difficult to use in the harsh conditions of many low-resource countries because of factors like heat and light sensitivity and the need for precise measurement. In these settings, amoxicillin dispersible tablets are a better option, particularly for children who can’t swallow pills. They have a longer shelf-life, are cost-effective, don’t need refrigeration, and are easy to administer because the tablets quickly disperse in clean water or breastmilk. Their lack of availability in countries where most needed, however, underscores the urgency of resolving barriers to access so these tablets can be put to work.

Cleaner-burning fuels can reduce indoor air pollution, which causes 4.3 million deaths—of which 12 percent are children with respiratory infections like pneumonia. Photo: PATH/Heng Chivoan.
4. Clean household fuels to clear the air
Nearly three billion people use coal, wood, and crop residue for cooking, but the smoke these fuels produce can cause serious illness. Indoor air pollution causes 4.3 million deaths, of which 12 percent are children with respiratory infections like pneumonia. Clean-burning fuel like liquid-petroleum gas is a potential solution, but it is often too costly for poor, rural communities. However, there are interventions streamlining supply chains, providing consumer financing, and using direct marketing to bring clean fuel into more households, but further investment is needed to maximize reach.

Thanks to a thriving human milk bank, an infant receives donor breastmilk in the neonatal intensive care unit at Mahila Chikitsalaya Government Hospital in Jaipur, India. Photo: PATH/Tom Furtwangler.
5. Human milk banking to protect vulnerable infants
Exclusive breastfeeding provides infants with the nutrients and hydration they need; prevents exposure to contaminated food and water that cause deadly illnesses like diarrhea; and confers protective antibodies against many illnesses, including pneumonia (a particularly dangerous infection for newborns). When infants don’t have access to their own mother’s milk, donor breastmilk is the next best thing. Human milk banks are an innovative solution that gives otherwise deprived infants access to safe donated breastmilk—and a chance to thrive.



